Addressing Gaps in Care:
CHD Patient Experience
UT Austin Design in Health Capstone
Team | Primary Investigators: Byron Wilson, Dr. Elizabeth McCollum, Dr. Andrew Wells Researchers: Ayesha Rahman, Iya Abdulkarim, Jewel Thompson-Adiuku, Claire Moreau, Veronica Remmert, Mara Fock, Emily McCalley, Shonta Brantford, Brooke Upchurch
SUMMARY
We developed a patient experience platform that would enhance the communication and understanding of the CHD care journey for families, patients and clinicians.
The Story
Congenital heart disease is a rare occurrence; 1/100 births newborns are affected by it. It is also a devastating occurrence; survivors of CHD are only now starting to make it to adulthood. These patients have been told their whole lives that survival and success in terms of their condition is slim. Now though, with these bettering survival rates, the goal of CHD patients’ health outcomes have gone from just living to living well.
“How (do we) enable patients to live full lives, to have goals?” - Dr. Wells, Dell Children’s Hospital
This lead to Project CORage, an effort to understand how to
Improve the lifelong journey of patients with CHD and their families.
The research team behind CORage utilized experience group research and in depth interviews to understand the lives of CHD patients beyond the moments of care. This led to the production of journey maps that detailed the phases of the lives of patients and the possible scenarios of each stage. Below is the lifelong journey map for an CHD patient:
Details on their approach can be found here.
The CORage study was able to identify the most meaningful outcomes (MMOs) to patients and families, categorized into:
capability (doing the things in life you want to)
comfort (experience of physical/emotional pain/distress)
calm (experiencing healthcare with the least impact on daily life)
They were also able to determine 27 gaps in care that were clustered into five themes:
Communication
Transitions across Life Stages
Patient and Family Support
Structural Deficiencies
Education
With this information gathered from CORage, there was now the question of:
What are the next steps?
My Role
Design Lead
Design Research
Synthesis
Co-creation and Prototyping
Service visualizations
What Are We Doing?
Our Design in Health research team has been gathered to determine those next steps. We are setting out to:
To validate the previous forms of qualitative research focused on gaining a better understanding of the life experiences and unmet needs of patients for the Texas Center for Pediatric and Congenital Heart Disease at UT Health Austin.
To qualitatively & quantitatively assess current clinician behaviors that contribute to positive elements of the (recently determined) patient journey.
Observations
We started our research process by conducting observations at Dell Children’s Hospital in Cardiac Care. Our team conducted observations through out the semester to garner information that would allow us to scope the research, get acclimated to the environment and learn what questions to ask.
I have had the opportunity to observe clinicians, staff, patients and families in:
Cardiac Care Unit
Cardiac Clinic
Catheter Lab
The operating room
The team gathering datapoints from observations to utilize in synthesis
Affinity Mapping
The KJ method was developed by Jiro Kawakita, an ethnologist. It became one of the seven management and planning tools in the 60s as part of the total quality management protocol.
Silent Observation Recordings: We took time to summarization all our observations from Miro onto Post-Its with single words or phrases without communication
Silent Affinity Mapping: We then, without talking, placed our observations on boards, near other ones that we thought related, slowly clustering what we had all seen together
Group Labelling: We then took time to give each category a label based on a theme we found within the group of observations
We utilized this affinity mapping method to create relationships between datapoints from our observations. We were able to identify broad themes that our team would later relate to the CORage findings.
we moved our observations to a physical medium to utilize a different part of our brains
What We Heard
CHD is a life transforming diagnosis
“You are basically living in the hospital... Whenever you are going through the process it is so traumatic”
“The doctor told me I needed to quit my job, so I did. They helped me with rent assistance”
It takes a huge team to treat it
“At one point I calculated how many doctors and nursed cared for my son over six months and it is insanely high. It feels like so many different people to communicate with...”
Gaps in team integration create friction
“Social status doesn’t help my medical diagnosis”
“I don’t think they know what we do day-to-day”
Opportunities for social-medical integration
“What if we gave the patient a notepad?”
“I get overwhelmed and I forget my questions”
“Where was he when I started social work school?”
Going Back to the Gaps in Care
After identifying themes from our observations, we juxtaposed those themes with the gaps found in the CORage study to support and confirm our findings through observations with findings from interviews.
“How Might We’s”
Now that we had completed our observations and cross referenced CORage, it was time to start moving into the design phase. We kicked this off through creating a brain storm space with “how might we’s”. We developed these three:
How might we standardize the communication between psychosocial team & medical team?
How might we strike a balance between expert & compassionate care in communication with patients?
How might we develop a standardized method for information streams for each patient?
Ideation
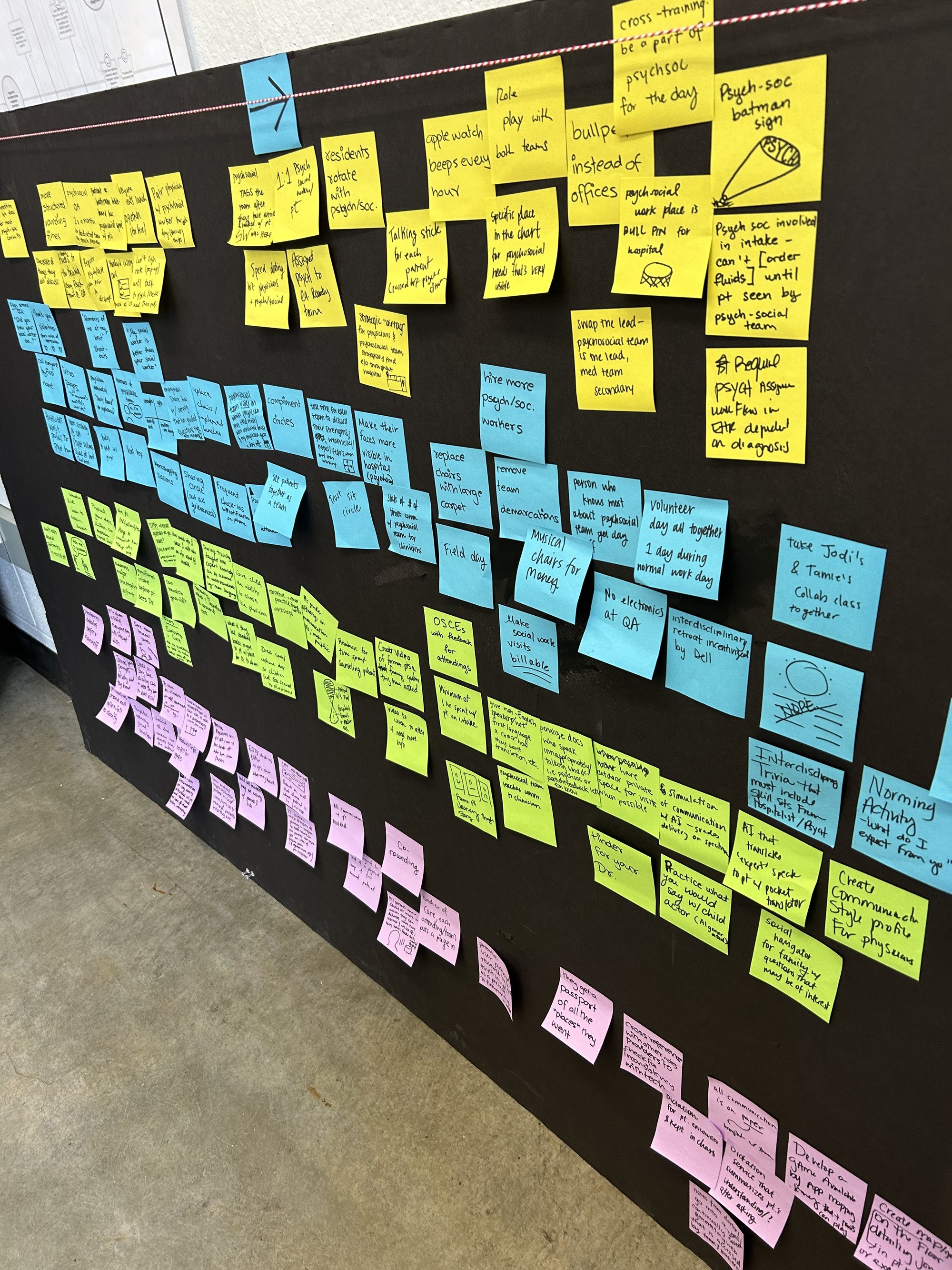
With these “how might we’s”, we moved into the ideation phase, where we developed over a 100 concepts, ranging from easy to impossible that we eventually consolidated and isolated to our final concept.
We then mapped these concepts to identify and understand where they might interact digitally and in real life with the care process.
We also referenced the primary research done in CORage again at this point to see if we could identify needs through quotes that related to the concepts we developed.
Though we would have liked to, our team did not get to complete interviews in our work on this project due to timeline and IRB protocol; so it then became very important for use to integrate and reference the primary research interviews done in the first phase of this project as well as our observations to support our design process.
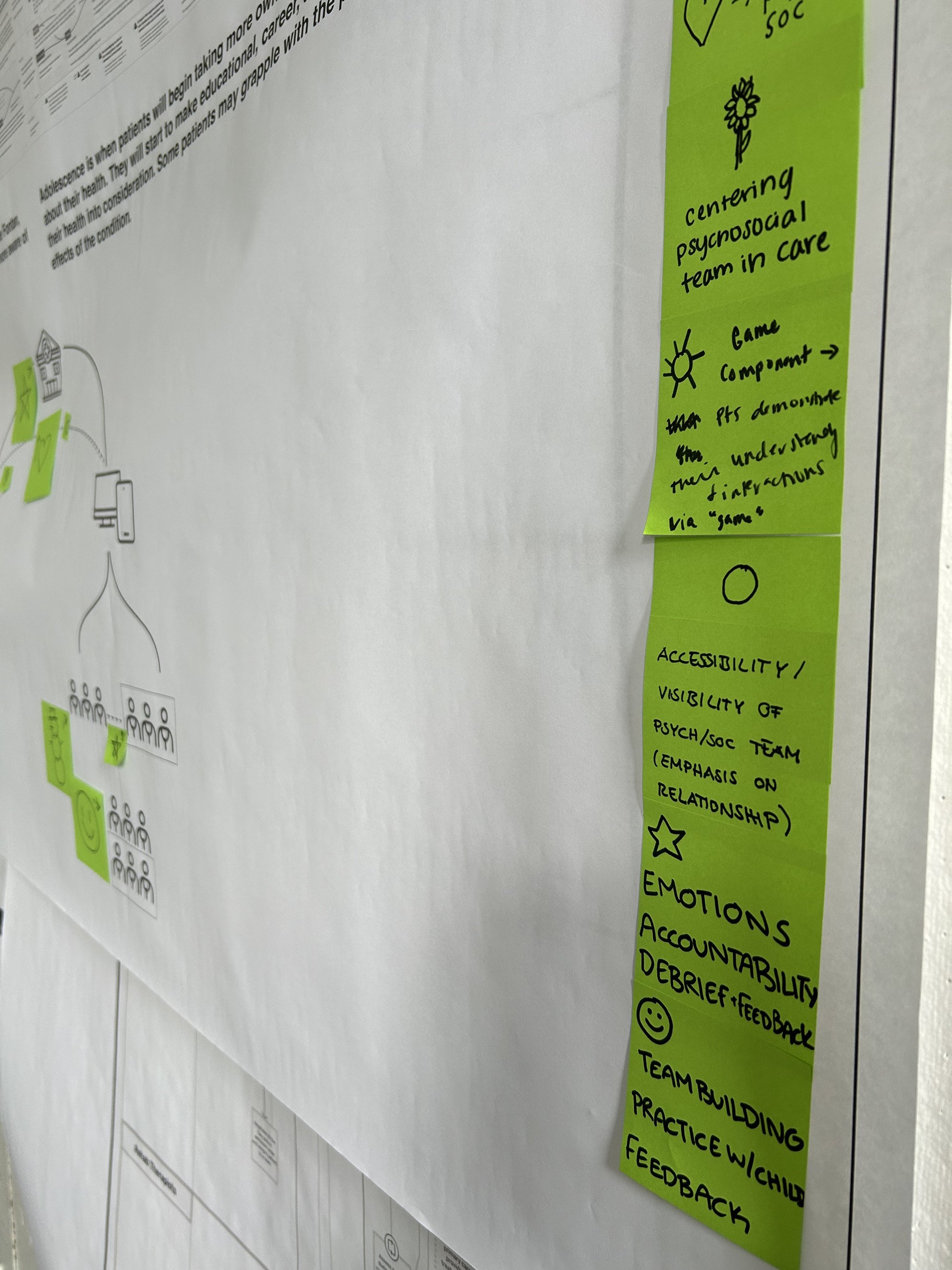
our ideation process with initial 100+ ideas
Final Prototype
Our final prototype was a patient experience platform for parents to utilize during their child’s care journey to address questions, worries and more. It would also track and display the progress of their in their SV-CHD journey. Through treatments, surgeries and life milestones, the platform would be utilized to communicate between clinicians and patient families.
There would also be a physical map for the patient to engage in their journey that mirrored the adult platform journey. It would be a way to engage young children in their care and celebrate their wins.
our service map depicting journey of patients, family and clinicians within the service; also depicts features and benefits.
Part of the service map depicted alongside the application interface to represent what that portion of the service would look like to users.